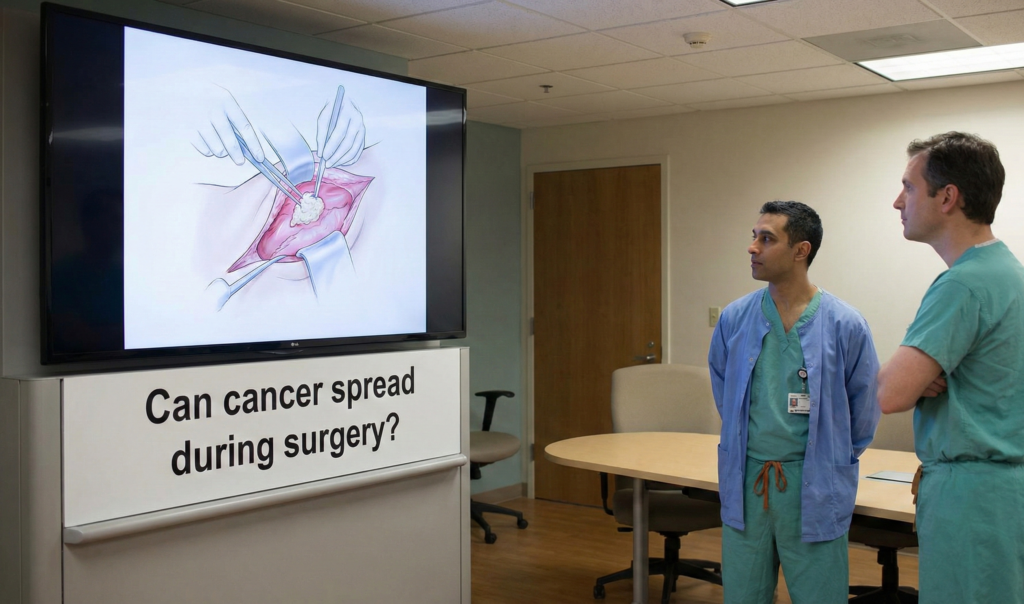
For anyone facing cancer surgery, fear and uncertainty are constant companions. Among the most unsettling questions is this: Could the surgery itself cause my cancer to spread? It’s a legitimate, deeply worrying concern. Today, we’ll separate myth from medical reality and explore what modern oncology knows about this possibility.
The Origin of the Fear: Understanding “Tumor Seeding”
The fear isn’t entirely unfounded. The concept is called “tumor seeding” or “iatrogenic spread,” where cancer cells might be dislodged during a biopsy or surgical procedure and take root in a new location.
Historically, this was a more significant risk with older techniques. Early surgeons had fewer tools to prevent the spillage of cells. This seeded the idea in public consciousness, sometimes amplified by anecdotal stories or outdated information.
The Modern Reality: What Does the Science Say?
The short answer is: The risk is extremely low with today’s standard surgical oncology practices, and the benefits of surgery almost always far outweigh this minimal risk.
Here’s why:
- Meticulous Surgical Techniques: Oncologic surgeons are trained in specific “no-touch” and en bloc resection techniques. This means they remove the tumor within a wide margin of healthy tissue, ideally without ever directly cutting into the cancerous mass. They handle only the healthy tissue around it.
- The “Biologic Barrier” Theory: Most cancer cells dislodged during surgery do not survive. They are damaged by the physical manipulation, lack a proper blood supply, and are attacked by the body’s immune system. To form a new tumor, they need to overcome immense biological hurdles.
- Advanced Technology: The use of laparoscopic (minimally invasive) surgery with specially designed containment bags for tumor removal has further reduced any risk of cells spreading into the incision site.
- Adjuvant Therapies: Often, surgery is just one part of the plan. Chemotherapy or radiation therapy before (neoadjuvant) or after (adjuvant) surgery is designed to eliminate any microscopic cancer cells that may have escaped, including those that might have been dislodged during the operation.
Are There Specific Concerns?
While rare, some scenarios have been studied more closely:
- Needle Biopsies: Fine-needle aspiration (FNA) for diagnosis carries a theoretical risk. However, studies show the track recurrence rate is exceedingly low (often less than 1%), and the critical diagnostic information gained is invaluable for planning correct treatment.
- Surgical Incision Sites: There are documented, but very rare, cases of cancer recurring along the surgical scar or tract. This is more commonly associated with certain cancer types (e.g., some abdominal or ovarian cancers) but remains an uncommon event overall.
- Body Cavity Spread: In cancers of the abdominal lining (like some advanced ovarian cancers), surgical disruption can theoretically spread cells within that cavity. Surgeons use extensive irrigation with sterile fluids to minimize this.
What Surgeons Do to Minimize Any Risk
Your surgical team employs a multi-layered defense:
- Changing Instruments and Gloves: After removing the tumor, surgeons often change gloves, gowns, and instruments before closing the wound to avoid “contaminating” the surgical site.
- Isolating the Tumor: Using pads, bags, and careful irrigation to contain any potential spillage.
- Margin Assessment: Ensuring a wide enough “margin” of healthy tissue is removed around the tumor.
- Multidisciplinary Planning: Your surgery is planned by a team including the surgeon, medical oncologist, and radiologist to sequence treatments in the most effective way.
The Critical Perspective: Why Surgery is Essential
It is vital to weigh the infinitesimally small risk of iatrogenic spread against the massive, proven benefit of removing the primary tumor. Surgery remains the most potent curative tool for most solid cancers. It reduces the tumor burden, can alleviate symptoms, and makes subsequent therapies more effective.
Delaying or refusing surgery out of fear of spread allows the known cancer to grow and metastasize on its own—a far greater and more likely danger.
What You Can Do: Empowered Patient Questions
Have this conversation with your surgeon. It will ease your mind. Ask:
- “What techniques will you use to minimize the risk of cancer cell spread during my procedure?”
- “Is my cancer type one where tract seeding is a noted consideration, and how do you address it?”
- “How will my surgery be integrated with other treatments (chemo/radiation) to address any microscopic disease?”
The Bottom Line
The idea that surgery routinely causes cancer to spread is largely a medical myth in the context of 21st-century cancer care. While biologically possible, the sophisticated techniques and protocols of modern surgical oncology have reduced this risk to a negligible level.
Trust in the science and the expertise of your team. The goal of cancer surgery is to cure you or significantly extend your life. By removing the primary tumor, your surgeon is taking the most decisive step toward that goal. Don’t let an outdated fear rob you of a potentially life-saving treatment.
Disclaimer: This blog is for informational purposes only and does not constitute medical advice. Always discuss your specific risks and benefits with your treating oncologist and surgeon.